Herniated Disc Disease
What is it?
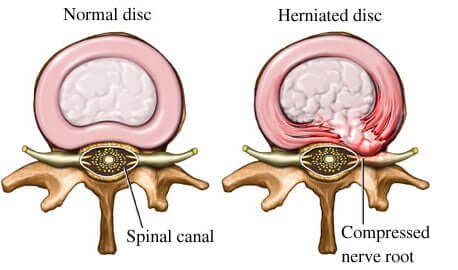
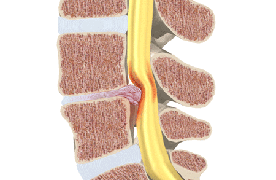
We have discs between each vertebra in our spine. They are made up of a fibrous outer ring, called the annulus fibrosus and a soft, gel like center, called the nucleus pulpous that serves as a shock absorber. A disc herniation occurs when there is leakage of the nucleus pulposus outside of the border of the annulus frequently causing back pain. A Disc herniation is usually due to age related degeneration of the annulus fibrosus, although trauma, lifting injuries, or straining can cause it as well. A Disc herniation is often the progression of a pre-existing disc “protrusion”, a condition in which the outermost layers of the annulus fibrosus are still intact, but can bulge when the disc is under pressure. In contrast to a herniation, none of the nucleus pulposus escapes beyond the outer layers in a disc protrusion. Many people have disc protrusions that do not cause back pain. It is possible to have a disc herniation that is not painful, if it does not press on any surrounding structures.
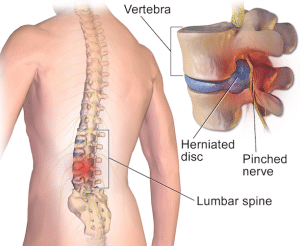
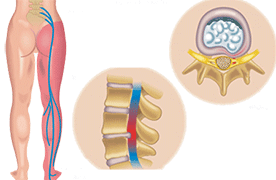
In a disc herniation, a tear in the fibrous outer ring allows the gel center to leak out. The leaking gel can cause a chemical inflammatory reaction to the surrounding tissue and nerves, which may directly cause back pain. The herniated disc can also press on nearby spinal nerves, causing severe back pain or even altered sensations such as numbness or tingling in an arm or leg. For instance, herniation of a lumbar disc can impinge (“pinch”) against a nerve of the legs, which can cause radiating pain from the back that travels down the leg to the foot. The pattern of the pain usually suggests which nerve is being pinched. In severe cases, a large disc herniation can press on nerves or even the spinal cord, resulting in weakness of arms or legs and possibly difficulty controlling urination or bowel function. If you have a severe back pain and loss of control of an extremity or of bowel or bladder function, you should go to an emergency room of a hospital that preferably has an MRI and a spine surgeon on call.
Video about Lumber Disc Herniation:
Who gets it?
A herniated disc is a common back injury and a common cause of back pain. It can happen to many different patient populations. Those who have experienced trauma can have a herniation, and this trauma can range from a car accident to a simple fall. Workers who lift heavy objects frequently are more at risk for a herniated disc because the weight tends to put pressure on the back, causing herniation. Lifting with poor posture, such as with a rounded back, can cause a disc herniation. Obese individuals also run a risk of stressing the back and prompting a spontaneous ruptured disc. Finally, discs become more brittle with age due to the progressive loss of water within. As patients become older, the discs degenerate, and they are more likely to herniate. Any area of the spine is susceptible to the effects of aging, and pain can occur anywhere along the spine. However, the majority of disc herniations occur in the lower back and the next most common site is the mid to lower neck.
What kind of pain results?
Two types of pain occur with disc herniation. The first is local pain, usually caused by the inciting injury. Soft tissue injury, muscle strains and sprains, and other localized pain can occur with disc herniations that indicate the back has been injured. Where disc herniations differ from more common soft tissue injury is in nerve involvement. Often, the herniation will press against nerves, and this will cause pain in all of the areas served by that nerve. For instance, a herniated disc in the neck might cause numbness, tingling, weakness, and pain in the arm. Similarly, a lumbar herniated disc causes tingling and numbness in the legs, called Sciatica. The pain tends to focus on one side or the other, depending on which side of the disc herniates, and the severity and extent of the nerve pain is dependent on the amount of impingement the nerve suffers. Pain can travel partly or all the way down an extremity.
Treatment
When back pain starts, most patients see their primary care provider for an initial workup. With radiographic images and a complete history and physical, these doctors can usually determine if the pain is simple soft tissue injury or if there may be nerve involvement suggesting a herniated disc.
Most of the time, pain from a herniated disc will improve with conservative measures: NSAIDs (Ibuprofen, Naproxen, etc), muscle relaxants, and physical therapy. Sometimes, judicial use of strong pain medications may be prescribed as needed to participate in physical therapy. However, if you are unable to participate in physical therapy due to severe pain or conservative treatment does not improve your pain in approximately six weeks, you should see a Pain Medicine physician. Likely, an MRI (Magnetic Resonance Imaging) will be ordered to image the discs and nerves of your spine. An MRI will reveal a herniated disc and any nerve impingement, if it is present. A Pain Medicine physician will provide you with guidelines to protect your back and allow healing. We have many treatment options that can successfully lower pain levels and improve your quality of life, such as restoring sleep. The goal of treatment is to lower pain levels so that you can return to physical therapy and move more normally. The treatment of choice is an epidural steroid injection with XRay guidance to place steroid, a strong anti-inflammatory agent, near the irritated nerve, thereby reducing pain and swelling. In addition, medications such as anti-seizure medications and anti-depressants can be used as well to reduce nerve pain.
We will explore many modalities, including back braces, TENS, and even alternative approaches to help improve your pain and restore your lifestyle. Should these measures fail to relieve pain, your Pain Medicine physician can recommend proceeding with surgery and will work with your primary care physician to refer you to a spine surgeon. Surgery is avoided in the majority of cases of a herniated disc.