Tendinopathy including Achilles tendonitis
What is it?
 Tendinopathy, or tendinitis, is a syndrome characterized by pain and dysfunction of a tendon, sometimes accompanied by swelling. Tendons are bands of fibrous connective tissue that connect muscles to bones. They are similar to ligaments, but these connect two different bones.
Tendinopathy, or tendinitis, is a syndrome characterized by pain and dysfunction of a tendon, sometimes accompanied by swelling. Tendons are bands of fibrous connective tissue that connect muscles to bones. They are similar to ligaments, but these connect two different bones.
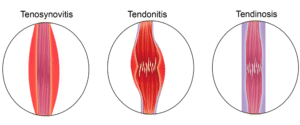
The term tendinopathy includes both tendon degeneration (tendinosis) and tendon dysfunction accompanied by inflammation (tendinitis). Tendinosis is mainly used to refer to the degenerative tissue changes in tendons that may or may not be painful and that are not associated with inflammation. The term tendinopathy specifically refers to painful tendon conditions, which are usually associated with tendon inflammation, at least in acute forms of tendinopathy. Tendinopathy is mainly due to overuse of tendons. Tendon injury is common during physical exercise, for example, when intense forces are exerted on tendons. Work-related repetitive movements are also a common source of tendinopathy.
Any tendon and its surrounding tissues can potentially undergo tendinopathy, with the most commonly affected tendons including the rotator cuff tendons (in the shoulders), elbow and wrist tendons, patella, tibial tendons, and the Achilles tendon. Of these, rotator cuff tendinopathy is the most common, with an incidence that greatly increases with age. The Achilles tendon, the largest and strongest tendon in the human body, is also frequently affected, most likely due to the load it is continuously subjected to, be it in everyday life or in most sports.
The diagnosis of tendinopathy is based on the characteristics of pain which is usually confined to a small area of the tendon, and on imaging studies (ultrasound, magnetic resonance imaging).
Tendinopathy is characterized as ‘acute’ when symptoms have been present for 0 to 6 weeks, as ‘sub-acute’ between 6 to 12 weeks, and as ‘chronic’ after more than 3 months.
Who gets it?
Tendon disorders occur frequently and may sometimes lead to significant disability and pain. Tendinopathy is highly prevalent in individuals whose occupation requires physical or repetitive work, such as in construction, food preparation and serving, transportation and material moving, and similar activities. The risk increases when there is a combination of force and exposure to vibration during repetitive tasks.
Sports-related injuries are another common cause of tendinopathies, particularly in the Achilles tendon. Achilles tendon ruptures occur frequently in athletes either due to an acute overload and trauma, or due to chronic degeneration.
In older individuals, rotator cuff tendinopathies are quite common; their incidence increases with age, affecting around 13% of individuals in their 50s, 25% of individuals in their 60s and 50% of individuals in their 80s.
What kind of pain results?
Acute tendinopathy pain is usually localized to a specific area of the tendon and has a transient nature closely linked to tendon loading. There is usually tenderness to touch and impaired function. While pain is transient, it is rarely experienced at rest or during low-load tendon use. In Achilles tendinopathy, pain is usually felt in the middle of the tendon, while in other tendinopathies pain is generally felt at either end of the tendon, at the insertion areas.
When pain becomes persistent, it is often intense and experienced even when there has been no loading on the tendon for a significant amount of time. Chronic tendinopathy may lose some of the inflammatory input present in acute tendinopathy and be the result of other sensitization mechanisms that have not been elucidated.
A characteristic pattern of tendinopathies is that when the tendon ‘warms up’ over the course of an activity, it becomes less painful; when it ‘cools down’, it may become very painful at variable times after activity. In some cases, pain can persist for years, for reasons that are not clearly understood and that make the management of pain more challenging.
Treatment of Tendinopathy
Since most tendinopathies are due to overuse, improvement may be achieved with rest, protection, stretching, and activity modification. However, that may not be applicable to patients with chronic tendinopathies.
When there is surgical repair of a tendon, tendon healing generally progresses through a short initial inflammatory phase, followed by a proliferative and a remodeling phase, which lasts for months.
Decreasing inflammation in the early stages following tendon repair may lead to improved healing. Non-steroidal anti-inflammatory drugs (NSAIDs) are widely used in the treatment of tendinopathies. Although they may be effective in acute, predominantly inflammatory tendinopathies, or in post-surgical inflammatory phases, their use in chronic tendon injuries is limited. Long-term use of NSAIDs is undesired, since it entails many risks, including an increased risk of gastrointestinal, cardiovascular, renal and hepatic diseases. These adverse effects are increasingly damaging as treatment time increases. Since chronic tendon injuries usually have long durations, NSAIDs may be counter-productive in those cases.
Corticosteroid injections are also frequently applied, and have also shown beneficial short-term effects, but longer-term pain relief through this approach is less easily achieved.
In the long-term, physical therapy designed for the specific type of tendinopathy may be useful, as well as other therapeutic modalities such as ultrasound, electrical stimulation, extra-corporeal shock wave therapy, or iontophoresis.


References
- Childress MA, Beutler A (2013). Management of chronic tendon injuries. Am Fam Physician, 87(7):486-90. PMID: 23547590
- Kaux JF, Forthomme B, Goff CL, Crielaard JM, Croisier JL (2011). Current opinions on tendinopathy. J Sports Sci Med, 10(2):238-53. PMID: 24149868
- Maffulli N, Wong J, Almekinders LC (2003). Types and epidemiology of tendinopathy. Clin Sports Med, 22(4):675-92. doi: 10.1016/S0278-5919(03)00004-8
- Rio E, Moseley L, Purdam C, Samiric T, Kidgell D, Pearce AJ, Jaberzadeh S, Cook J (2014). The pain of tendinopathy: physiological or pathophysiological? Sports Med, 44(1):9-23. doi: 10.1007/s40279-013-0096-z
- Thomopoulos S, Parks WC, Rifkin DB, Derwin KA (2015). Mechanisms of tendon injury and repair. J Orthop Res, 33(6):832-9. doi: 10.1002/jor.22806