Cervicalgia (Neck Pain)
What is Neck pain?
Cervicalgia is a general term used to describe pain in the neck. Neck pain is not a condition, but a symptom that can result from many different causes. Treating neck pain is highly dependent on having an accurate diagnosis. Examples of common conditions causing neck pain are neck strain, degenerative disc disease, neck injury such as whiplash, a herniated disc, or a pinched nerve.
Who gets it?
All persons are at risk for neck pain or injury. It is estimated that nearly two thirds of the population will experience neck pain at some point in their lives. Risk factors for neck pain include injury from involvement in contact sports, motor-vehicle accidents, poor postures or sleeping positions, psychological stress, and advance age. Whiplash is almost always caused by trauma of some kind. Usually a rear end car collision is the classic example of the inciting incident for this type of neck pain.

What kind of pain results?
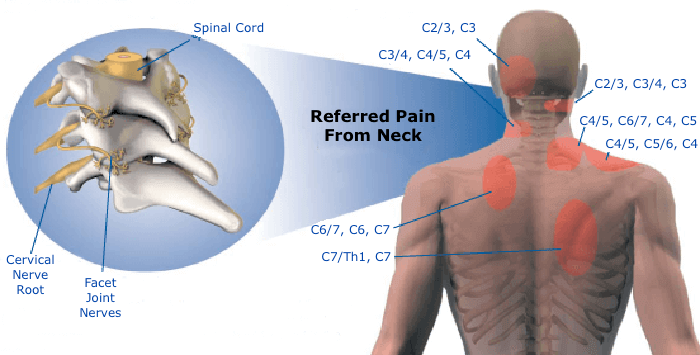
Neck pain can present in different ways, depending on the cause and structures involved. Neck pain is commonly associated with dull aching localized to the neck. At times the pain can worsen with movement of the neck or turning of the head. Other symptoms that are associated with some forms of neck pain include numbness, tingling, sharp or shooting pain. Neck pain can also be associated with headache, facial pain, or shoulder pain. These associated symptoms are often a result of pinched or irritated nerves in the neck. Neck pain can also be accompanied by upper and or lower back pain in some conditions.
What is Whiplash?
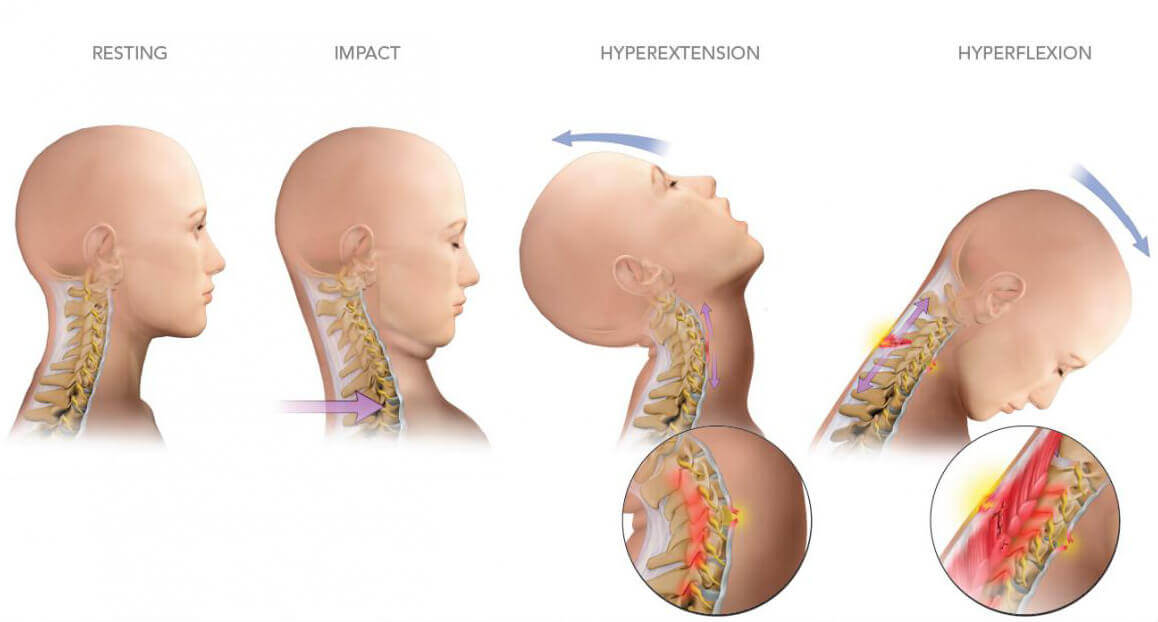
One of the most common forms of neck pain is whiplash, and it is distinct from cervicalgia and other causes of neck pain. Whiplash is primarily a soft tissue injury to the neck. When the head is whipped forward and back quickly and violently, the ligaments and supportive musculature become overextended.
Treatment of Neck Pain
Management of neck pain often start with conservative measures and treatment modalities. Conservative measures are often satisfactory in the treatment of whiplash pain. The condition can be temporary and may not last beyond a few weeks. However, some patient’s experience the pain of this condition for an extended period of time following the incident or injury, and in those cases more aggressive treatment is needed.
Whiplash that does not respond to conservative treatments can be treated with cervical facet injections. Physical therapy, heat, ice, and use of over the counter analgesic medications can treat symptoms related to soft tissue injury, muscle strain or symptoms of whiplash. In some cases of whiplash an immobilization collar is used, however this practice remains controversial. Supporting the structures of the neck with a collar may lead to deconditioning and potential atrophy of the muscles of the neck, which can lead to additional pain symptoms and lengthened recovery time. Your pain physician will evaluate you and help you decide which treatment will be most effective for you. When your neck pain is reduced with medications or interventional procedures as described above, it is common practice to repeat physical therapy. Doing so will help restore muscle strength and movement, and ultimately help you return to your previous level of functioning. When conservative measures are less than effective, or a diagnosis is uncertain, a patient should be referred to a pain management specialist for evaluation and alternative treatment options. Once a diagnosis is made, the pain management physician will then determine the appropriate treatment for the pain syndrome. Treatments can include medication management and, or procedural interventions.
Pain caused by muscle spasm in the neck, shoulders, or upper back regions, also known as myofascial pain can be treated with injections called trigger point injections. Trigger point injections involve injecting a solution of local anesthetic and steroid directly into the muscle. This injection helps to relieve muscular pain by reducing inflammation and relaxing the muscle. If the trigger point injections reduce the pain but only for a short period of time (days to weeks) an injection of Botox A can be injected into the spastic muscles. Botox A is a protein derived from the organism that causes botulism, however it is not live and when injected appropriately into spastic muscles it weakens then enough to allow softening of the muscle, improved movement and reduced pain. Botox A has an effect for three months and can be repeatedly injected, often in three month intervals, as needed. (See Botox A)
When pain results from a herniated disc or pinched nerve and is associated with radiating pain into the upper extremities a local anesthetic and steroid solution can be injected into the epidural space at the level of the disc dysfunction. This is known as a cervical epidural steroid injection, and is done under fluoroscopic (or X-Ray) guidance. These injections are considered a series of three, with one injection per month for three months, and can offer anywhere from a few weeks to several months of pain relief.
Pain caused by arthritis of the joints in the cervical spine (facet joints) can be treated with cervical facet joint injections, also known as medial branch blocks. This type of injection procedure is also done under fluoroscopic guidance. It works by blocking the nerve signals from the facet joints of the cervical spine and can relieve pain and allow for improved movement of the neck. If a patient experiences greater than 50% improvement in their pain with two consecutive injections spaced one month apart, subsequent treatment regimen includes radiofrequency ablation of the cervical facet joints. This procedure involves burning of the nerves that arise from the facet joints of the cervical spine and can offer 6-8 months of relief.
Don’t Suffer Any Longer…