Chronic Post Surgical Pain
What is it?
Chronic post-surgical pain is defined as pain that develops after surgery and lasts for more than two months. To be diagnosed as such, other possible causes of pain have to be excluded, namely any conditions preceding the surgery.
A surgical incision produces tissue injury, inflammation, and, consequently, pain. Acute post-surgical pain is therefore a normal physiological response to the damage induced to tissues. However, this pain should subside after healing is complete. But this is not always the case. In many patients, chronic pain ensues. Some patients may actually be pain-free or have only mild pain in the acute post-surgical period, with more intense pain developing only weeks or even months after surgery.
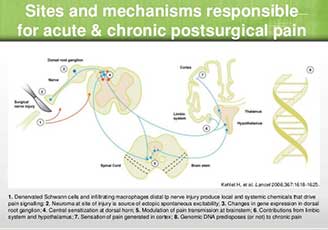
The development of chronic post-surgical pain is attributed to changes in the peripheral and central nervous system arising as a consequence of nerve injury and/or inflammation.
Thoracic surgeries including thoracotomy or mastectomy are some of the highest risk procedures in what concerns chronic post-surgical pain. This may be due to the fact that extensive nerve damage is frequent in thoracotomy, and occasionally reported in mastectomy. Chemotherapy and radiotherapy can also induce neuropathic pain, which may also explain the high incidence of chronic pain after mastectomy.

Who gets it?
Anyone who undergoes a major surgery is potentially at risk of developing chronic post-surgical pain. Epidemiological studies show widely variable prevalence estimates. On average, between 10 and 30% of patients who undergo common surgical procedures report persistent or intermittent pain of varying severity one year after surgery. The rate is higher for major thoracic surgeries: up to 40% of patients may develop chronic pain. Pain can be severe, or even disabling, in 5 to 10% of patients.
There are a few risk factors that may predict the development of chronic post-surgical pain. The presence of pre-surgical pain is often associated with the development of post-surgical pain; age may also contribute, since younger patients seem more prone to develop post-surgical pain; genetic predisposition and psychological factors, such as anxiety, vulnerability or resilience, can also determine the susceptibility to developing post-surgical pain.
The procedure itself is also a key determinant of the likelihood of developing post-surgical pain, specifically the surgical technique, the type of anesthesia, the inflammatory response to tissue damage, and possible nerve damage during surgery, which may result from transection, stretching, contusion, crushing, entrapment or compression of nerves, for example.
Overall, the development of chronic post-surgical pain is most likely due to a combination of these factors.
What kind of pain results?
Chronic post-surgical pain usually lasts for more than 3 to 6 months after surgery. It may be the result either of unresolved inflammation or of neuropathy due to nerve injury induced by the surgery.
Immediately after surgery, there may be pain and increased sensitivity to movement and touch at the site of surgery and at the tissues surrounding it. If nerve injury occurred during surgery, neuropathic pain may develop. Features of neuropathic pain include sensory abnormalities, increased reaction to painful stimuli (hyperalgesia), and pain in response to previously non-painful stimuli, such as touch (allodynia). This is observed in most patients with chronic post-surgical pain. The intensity of chronic pain will also depend on the who gets it.
Anyone who undergoes a major surgery is potentially at risk of developing chronic post-surgical pain. Epidemiological studies show widely variable prevalence estimates. On average, between 10 and 30% of patients who undergo common surgical procedures report persistent or intermittent pain of varying severity one year after surgery. The rate is higher for major thoracic surgeries: up to 40% of patients may develop chronic pain. Pain can be severe, or even disabling, in 5 to 10% of patients.
There are a few risk factors that may predict the development of chronic post-surgical pain. The presence of pre-surgical pain is often associated with the development of post-surgical pain; age may also contribute, since younger patients seem more prone to develop post-surgical pain; genetic predisposition and psychological factors, such as anxiety, vulnerability or resilience, can also determine the susceptibility to developing post-surgical pain.
The procedure itself is also a key determinant of the likelihood of developing post-surgical pain, specifically the surgical technique, the type of anesthesia, the inflammatory and any nerve damage during surgery. Overall, the development of chronic post-surgical pain is most likely due to a combination of these factors.
Although post-surgical pain is predominantly felt at and around the site of injury, when it becomes chronic it may radiate to more distal tissues. Post-thoracotomy and post-mastectomy pain may be felt in the chest, arm, axilla and shoulder regions. The pain is primarily described as tenderness, tightness, pulling/dragging sensations and numbness, but it is also commonly felt as burning or stabbing pain.
Treatment of chronic post-surgical pain
In the acute phase, opioids and non-steroidal anti-inflammatory drugs (NSAIDs) have good efficacy. But as chronic pain develops, pain treatment becomes less effective. In order to determine the best approach, it must be assessed whether pain has a predominantly inflammatory or neuropathic origin. If neuropathic pain develops, it will most likely be resistant to anti-inflammatory drugs. It is also possible that pain may be a result of both inflammation and neuropathy.
Opioids such as morphine, fentanyl or oxycodone remain the first line of treatment for post-surgical pain, despite their wide array of side-effects, such as nausea, sedation, vomiting and respiratory deficits. NSAIDs are generally inadequate as the sole analgesic drug for severe post-surgical pain. However, a combined therapy using NSAIDs and opioids may decrease the intensity of post-surgical pain while simultaneously decreasing the doses of opioids required, and thereby decreasing undesired opioid side-effects.
Antidepressants are also useful for patients with neuropathic pain, even when patients have not been diagnosed with depression. Tricyclic antidepressants, such as amitriptyline and nortriptyline, seem to be more effective than selective serotonin reuptake inhibitors, such as duloxetine and desvenlafaxine.
Anticonvulsant drugs, such as gabapentin, pregabalin and carbamazepine, are effective in a number of neuropathic pain conditions and have also shown efficacy in chronic post-surgical pain. A combined therapy with opioids may also be effective and decrease the doses of opioids used.
Combination therapies with corticosteroids, namely dexamethasone, may also reduce post-surgical pain while, again, decreasing opioid consumption; dexamethasone also reduces nausea and vomiting.
Overall, the best treatment chronic post-surgical pain may be a personalized multimodal approach using a combination of drugs or other techniques, such as transcutaneous electrical nerve stimulation (TENS), for example. This may allow an effective targeting of multiple sources and mechanisms of chronic post-surgical pain.



References
- Bruce J, Quinlan J (2011). Chronic Post Surgical Pain. Rev Pain, 5(3):23–29. doi: 10.1177/204946371100500306
- Haroutiunian S, Nikolajsen L, Finnerup NB, Jensen TS (2013). The neuropathic component in persistent postsurgical pain: a systematic literature review. Pain, 154(1):95-102. doi: 10.1016/j.pain.2012.09.010
- Kehlet H, Jensen TS, Woolf CJ (2006). Persistent postsurgical pain: risk factors and prevention. Lancet, 367(9522):1618-25. doi: 10.1016/S0140-6736(06)68700-X
- Macrae WA, Davies HTO. Chronic postsurgical pain. In: Crombie IK, editor. ed. Epidemiology of pain. Seattle: IASP Press; 1999:125–42.
- Van de Ven TJ, John Hsia HL (2012). Causes and prevention of chronic postsurgical pain. Curr Opin Crit Care, 18(4):366-71. doi: 10.1097/MCC.0b013e3283557a7f
- Lovich-Sapola J, Smith CE, Brandt CP (2015). Postoperative pain control. Surg Clin North Am, 95(2):301-18. doi: 10.1016/j.suc.2014.10.002
- Steyaert A, De Kock M (2012). Chronic postsurgical pain. Curr Opin Anaesthesiol, 25(5):584-8. doi: 10.1097/ACO.0b013e32835743b7